Alkahtani S.A., King N.A., Hills A.P., Byrne N.M. (2013) Effect of interval training intensity on fat oxidation, blood lactate and the rate of perceived exertion in obese men. SpringerPlus 2, 532. |
 American Diabetes Association (2015) Classification and Diagnosis of Diabetes. Diabetes Care 38, S8-S16. |
 Arad A.D., DiMenna F.J., Thomas N., Tamis-Holland J., Weil R., Geliebter A., Albu J.B. (2015) High-intensity interval training without weight loss improves exercise but not basal or insulin-induced metabolism in overweight/obese African American women. Journal of Applied Physiology 119, 352-362. |
 Astorino T.A., Schubert M.M., Palumbo E., Stirling D., McMillan D.W. (2013) Effect of two doses of interval training on maximal fat oxidation in sedentary women. Medicine & Science in Sports & Exercise 45, 1878-1886. |
 Bouchard C., Church T.S., Earnest J.M., Häkkinen K., Jenkins N.T., Karavirta L., Kraus W.E., Leon A.S., Rao D.C., Sarzynski M.A., Skinner J.S., Slentz C.A., Rankinen T., Li S. (2012) Adverse metabolic response to regular exercise: is it a rare or common occurrence?. PLoS ONE 7, e37887. |
 Braun B., Sharoff C., Chipkin S.R., Beaudoin F. (2004) Effects of insulin resistance on substrate utilization during exercise in overweight women. Journal of Applied Physiology 97, 991-997. |
 Bülow J., Gjeraa K., Enevoldsen L.H., Simonsen L. (2006) Lipid mobilization from human abdominal, subcutaneous adipose tissue is independent of sex during steady-state exercise. Clinical Physiology and Functional Imaging 26, 205-211. |
 Burgomaster K.A., Howarth K.R., Phillips S.M., Rakobowchuk M., MacDonald M.J., McGee S.L., Gibala M.J. (2008) Similar metabolic adaptations during exercise after low volume sprint interval and traditional endurance training in humans: metabolic adaptations to sprint or endurance training in humans. The Journal of Physiology 586, 151-160. |
 Corpeleijn E., Mensink M., Kooi M.E., Roekaerts P.M.H.J., Saris W.H.M., Blaak E.E. (2008) Impaired skeletal muscle substrate oxidation in glucose-intolerant men improves after weight loss. Obesity 16, 1025-1032. |
 Cowan T.E., Brennan A.M., Stotz P.J., Clarke J., Lamarche B., Ross R. (2018) Separate effects of exercise amount and intensity on adipose tissue and skeletal muscle mass in adults with abdominal obesity. Obesity 26, 1696-1703. |
 Crampes F., Marion-Latard F., Zakaroff-Girard A., de Glisenzinski I., Harant I., Thalamas C., Stich V., Rivière D., Lafontan M., Berlan M. (2003) Effects of a longitudinal training program on responses to exercise in overweight men. Obesity Research 11, 247-256. |
 Daussin F.N., Zoll J., Dufour S.P., Ponsot E., Lonsdorfer-Wolf E., Doutreleau S., Mettauer B., Piquard F., Geny B., Richard R. (2008) Effect of interval versus continuous training on cardiorespiratory and mitochondrial functions: relationship to aerobic performance improvements in sedentary subjects. American Journal of Physiology: Regulatory, Integrative and Comparative Physiology 295, R264-R272. |
 Fabbri E., Chia C.W., Spencer R.G., Fishbein K.W., Reiter D.A., Cameron D., Zane A.C., Moore Z.A., Gonzalez-Freire M., Zoli M., Studenski S.A., Kalyani R.R., Egan J.M., Ferrucci L. (2016) Insulin resistance is associated with reduced mitochondrial oxidative capacity measured by 31P magnetic resonance spectroscopy in non-diabetic participants from the Baltimore Longitudinal Study of Aging. Diabetes 66, 170-176. |
 Friedlander A.L., Casazza G.A., Horning M.A., Huie M.J., Brooks G.A. (1997) Training-induced alterations of glucose flux in men. Journal of Applied Physiology 82, 1360-1369. |
 Friedlander A.L., Casazza G.A., Horning M.A., Buddinger T.F., Brooks G.A. (1998) Effects of exercise intensity and training on lipid metabolism in young women. American Journal of Physiology: Endocrinology and Metabolism 275, E853-863. |
 Friedlander A.L., Casazza G.A., Horning M.A., Huie M.J., Piacentini M.F., Trimmer J.K., Brooks G.A. (1998) Training-induced alterations of carbohydrate metabolism in women: women respond differently from men. Journal of Applied Physiology 85, 1175-1186. |
 Gilbertson N.M., Eichner N.Z.M., Francois M., Gaitán J.M., Heiston E.M., Weltman A., Malin S.K. (2018) Glucose tolerance is linked to post-prandial fuel use independent of exercise dose. Medicine & Science in Sports & Exercise 50, 2058-2066. |
 Goodpaster B.H., Katsariaras A., Kelley D.E. (2003) Enhanced fat oxidation through physical activity is associated with improvements in insulin sensitivity in obesity. Diabetes 52, 2191-2197. |
 Hazell T.J., Olver T.D., Hamilton C.D., Lemon P.W.R. (2012) Two minutes of sprint-interval exercise elicits 24-hr oxygen consumption similar to that of 30 min of continuous endurance exercise. International Journal of Sport Nutrition and Exercise Metabolism 22, 276-283. |
 Hood M.S., Little J.P., Tarnopolsky M.A., Myslik F., Gibala M.J. (2011) Low-volume interval training improves muscle oxidative capacity in sedentary adults. Medicine & Science in Sports & Exercise 43, 1849-1856. |
 Huang Y., Cai X., Mai W., Li M., Hu Y. (2016) Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. The British Medical Journal 355, i5953. |
 Kuo C.C., Fattor J.A., Henderson G.C., Brooks G.A. (2005) Lipid oxidation in fit young adults during postexercise recovery. Journal of Applied Physiology 99, 349-356. |
 Lanzi S., Codecasa F., Cornacchia M., Maestrini S., Capodaglio P., Brunani A., Fanari P., Salvadori A., Malatesta D. (2015) Short-term HIIT and Fat training increase aerobic and metabolic fitness in men with class II and III obesity: exercise training in severe obesity. Obesity 23, 1987-1994. |
 Little J.P., Safdar A., Wilkin G.P., Tarnopolsky M.A., Gibala M.J. (2010) A practical model of low-volume high-intensity interval training induces mitochondrial biogenesis in human skeletal muscle: potential mechanisms. The Journal of Physiology 588, 1011-1022. |
 Little J.P., Gillen J.B., Percival M.E., Safdar A., Tarnopolsky M.A., Punthakee Z., Jung M.E., Gibala M.J. (2011) Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. Journal of Applied Physiology 111, 1554-1560. |
 Malin S.K., Haus J.M., Solomon T.P.J., Blaszczak A., Kashyap S.R., Kirwan J.P. (2013) Insulin sensitivity and metabolic flexibility following exercise training among different obese insulin-resistant phenotypes. American Journal of Physiology: Endocrinology and Metabolism 305, E1292-E1298. |
 Malin S.K., Viskochil R., Oliver C., Braun B. (2013) Mild fasting hyperglycemia shifts fuel reliance toward fat during exercise in adults with impaired glucose tolerance. Journal of Applied Physiology 115, 78-83. |
 Malin S.K., Braun B. (2013) Effect of metformin on substrate utilization after exercise training in adults with impaired glucose tolerance. Applied Physiology, Nutrition, and Metabolism 38, 427-430. |
 Meex R.C.R., Schrauwen-Hinderling V.B., Moonen-Kornips E., Schaart G., Mensink M., Phielix E., van de Weijer T., Sels J-P., Schrauwen P., Hesselink M.K.C. (2010) Restoration of Muscle Mitochondrial Function and Metabolic Flexibility in Type 2 Diabetes by Exercise Training Is Paralleled by Increased Myocellular Fat Storage and Improved Insulin Sensitivity. Diabetes 59, 572-579. |
 Ogurtsova K., da Rocha F.J.D., Huang Y., Linnenkamp U., Guariguata L., Cho N.H., Cavan D., Shaw J.E., Makaroff L.E. (2017) IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Research and Clinical Practice 128, 40-50. |
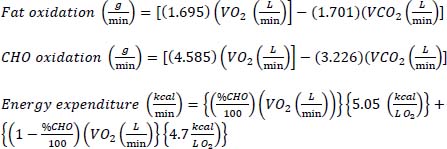
 Peronnet F., Massicotte D. (1991) Table of nonprotein respiratory quotient: an update. Canadian Journal of Sport Sciences 16, 23-29. |
 Prior S.J., Ryan A.S., Stevenson T.G., Goldberg A.P. (2014) Metabolic inflexibility during submaximal aerobic exercise is associated with glucose intolerance in obese older adults: metabolic inflexibility during exercise in IGT. Obesity 22, 451-457. |
 Pruchnic R., Katsariaras A., He J., Kelley D.E., Winters C., Goodpaster B.H. (2004) Exercise training increases intramyocellular lipid and oxidative capacity in older adults. American Journal of Physiology: Endocrinology and Metabolism 287, E857-E862. |
 Saris W.H., Schrauwen P. (2004) Substrate oxidation differences between high- and low-intensity exercise are compensated over 24 hours in obese men. International Journal of Obesity 28, 759-765. |
 Skleryk J.R., Karagounis L.G., Hawley J.A., Sharman M.J., Laursen P.B., Watson G. (2013) Two weeks of reduced-volume sprint interval or traditional exercise training does not improve metabolic functioning in sedentary obese men. Diabetes, Obesity and Metabolism 15, 1146-1153. |
 Solomon T.P.J., Sistrun S.N., Krishnan R.K., Del Aguila L.F., Marchetti C.M., O'Carroll S.M., O'Leary V.B., Kirwan J.P. (2008) Exercise and diet enhance fat oxidation and reduce insulin resistance in older obese adults. Journal of Applied Physiology 104, 1313-1319. |
 Talanian J.L., Galloway S.D.R., Heigenhauser G.J.F, Bonen A., Spriet L.L. (2006) Two weeks of high-intensity aerobic interval training increases the capacity for fat oxidation during exercise in women. Journal of Applied Physiology 102, 1439-1447. |
 Tsujimoto T., Sasai H., Miyashita M., Eto M., So R., Ohkubo H., Tanaka K. (2012) Effect of weight loss on maximal fat oxidation rate in obese men. Obesity Research & Clinical Practice 6, e111-e119. |
 Van Aggel-Leijssen D.P.C., Saris W.H.M., Wagenmakers A.J.M., Senden J.M., Van Baak M.A. (2002) Effect of exercise training at different intensities on fat metabolism of obese men. Journal of Applied Physiology 92, 1300-1309. |
 Venables M.C., Jeukendrup A.E. (2008) Endurance Training and Obesity: Effect on Substrate Metabolism and Insulin Sensitivity. Medicine & Science in Sports & Exercise 40, 495-502. |
|